Kenya has been officially validated by the World Health Organisation (WHO) as having eliminated human African trypanosomiasis (HAT), also known as sleeping sickness, as a public health problem.
This makes Kenya the second country in Africa, after Rwanda, to achieve this milestone and the tenth globally.
HAT is a neglected tropical disease (NTD) caused by the blood parasite Trypanosoma brucei rhodesiense, transmitted by tsetse flies. It is fatal within weeks if untreated, as the parasite invades multiple organs, including the brain.
In Kenya, the disease once threatened communities in Busia, Bungoma, Homabay, Siaya, Migori and Narok counties but the country has not reported any indigenous cases since 2009.
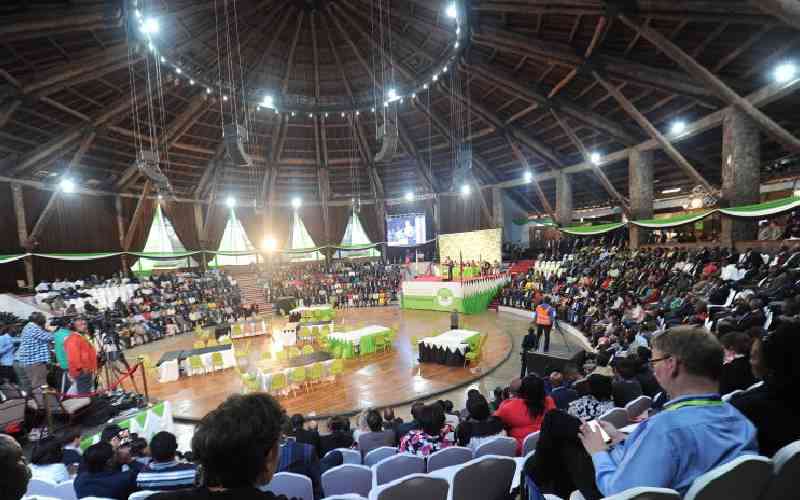
Speaking at the celebration event in Nairobi, WHO Representative Dr Adiele Onyeze congratulated Kenya for its determination.
“This is a significant day for public health. It shows what is possible when governments, communities and partners work together towards a shared goal,” he said.
Director General for Health Dr Patrick Amoth described the validation as a “key milestone” for the country.
“This reflects Kenya’s commitment over many years, through collaboration between national and county governments, research institutions, development partners and the communities themselves,” he said.
“The country remains fully committed to sustain the quality of care and surveillance in line with WHO’s recommendations.”
Dr Ndirangu Wanjuki, Country Director for Amref Health Africa, praised the power of collaboration and the ‘One Health’ approach, which integrates human, animal and environmental health.
“Nobody can do it alone, and we truly appreciate the leadership from the Ministry of Health,” he said. “These achievements give us immense hope, showing that it is possible to relieve the suffering of the most vulnerable in our society.”
From the research and innovation side, Prof Sam Kariuki, Continental Lead Africa and Eastern Africa Director at the Drugs for Neglected Diseases initiative (DNDi), said new treatment options had transformed the fight against HAT.
“We are very proud to have contributed to the development of a safe, effective and easy-to-administer oral treatment that has replaced toxic, arsenic-based drugs,” he said.
Principal Secretary for Public Health and Professional Standards Mary Muthoni termed the elimination of the disease “a watershed milestone” in Kenya’s health journey.
Stay informed. Subscribe to our newsletter
“This achievement underscores our conviction that universal health coverage anchored in primary health care can transform health outcomes for all Kenyans,” she said.
The Ministry of Health, in the press release, hailed the elimination as “more than a technical milestone.” In a statement, the ministry said: “It’s a triumph for the people of Kenya, especially our communities in the Lake Region who for generations lived with the constant threat of this disease. This follows many years of dedication, hard work and collaboration.”
According to WHO, Kenya strengthened surveillance in 12 health facilities across six historically endemic counties, equipping them with modern diagnostic tools and training staff. The country also stepped up monitoring of tsetse fly populations and animal trypanosomiasis through the Kenya Tsetse and Trypanosomiasis Eradication Council.
WHO Director-General Dr Tedros Adhanom Ghebreyesus also sent his congratulations: “Kenya joins the growing ranks of countries freeing their populations of human African trypanosomiasis. This is another step towards making Africa free of neglected tropical diseases.”
Globally, 57 countries have eliminated at least one NTD, and 10, including Kenya, have now eliminated sleeping sickness as a public health problem. The other nations are Benin, Chad, Côte d’Ivoire, Equatorial Guinea, Ghana, Guinea, Rwanda, Togo and Uganda.
Dr Onyeze urged vigilance even after elimination. “We encourage all stakeholders to remain involved in post-validation monitoring,” he said. Kenya’s post-validation plan includes continued surveillance, early detection, vector control and integration of HAT services into routine public health systems.
Prof Kariuki noted that the work is not over: “We remain committed to supporting countries across Africa to eliminate sleeping sickness for good.”